Table of Contents
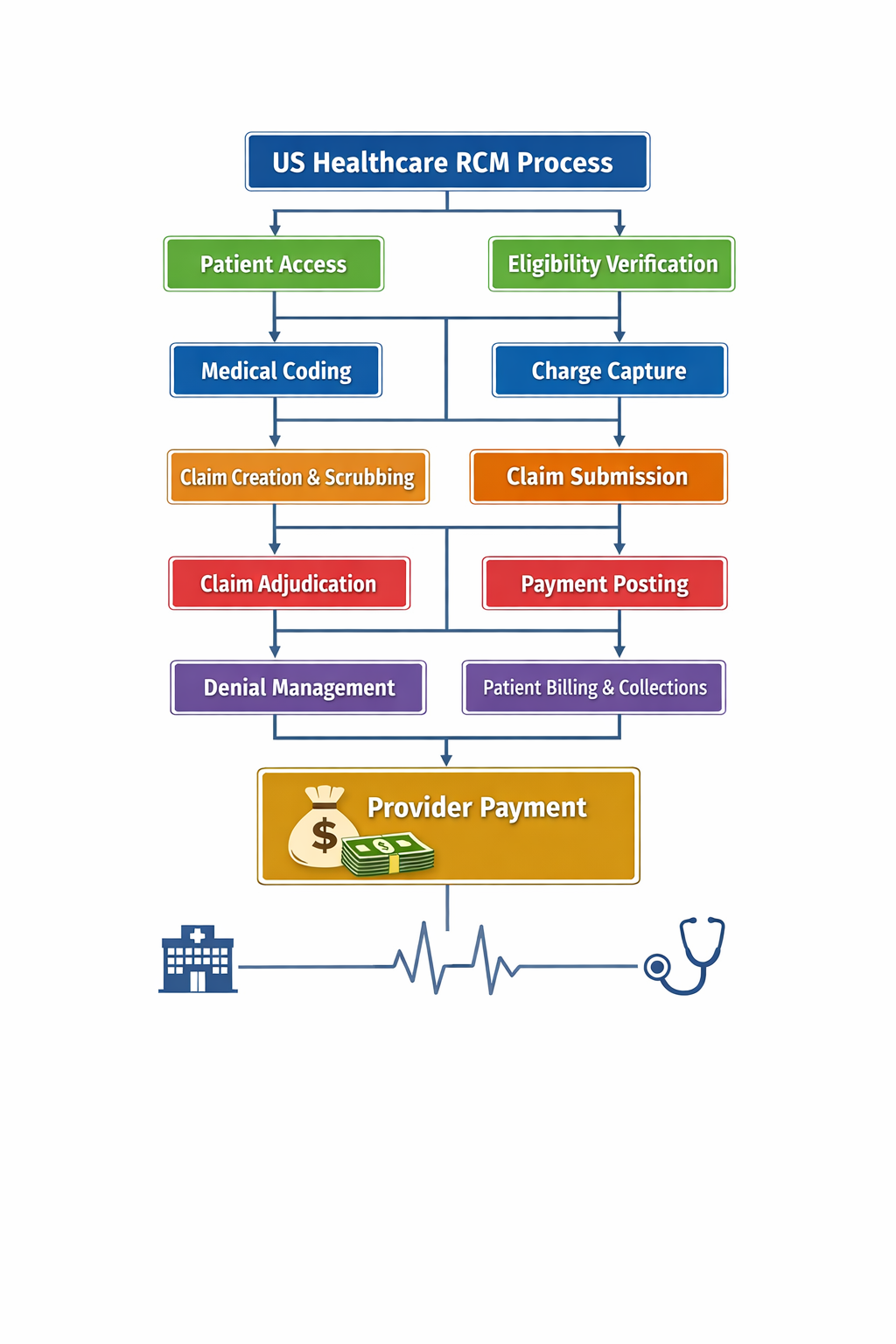
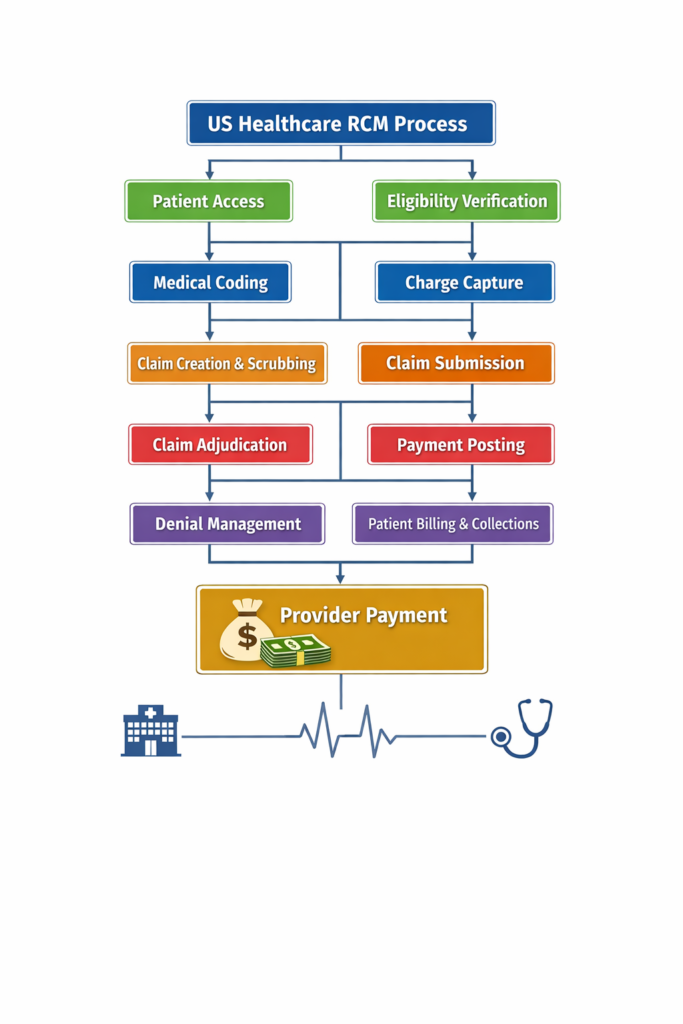
The US Healthcare RCM (Revenue Cycle Management) process is the financial backbone of hospitals, clinics, and physician practices in the United States. It controls how healthcare providers capture revenue, reduce denials, and maintain healthy cash flow. A single error at any stage can delay or completely stop payment. Understanding US Healthcare RCM from start to finish is essential for medical coders, billers, providers, and healthcare administrators. This guide explains every stage clearly—from patient entry to final payment—using practical terms and real-world workflow logic.
Stage 1: Patient Access in US Healthcare RCM
Patient access is the foundation of US Healthcare RCM. This stage begins before the patient even meets the doctor. Accurate patient demographics, insurance details, and contact information are collected. Errors here create downstream claim rejections and payment delays.
Front-end accuracy is a power move in revenue protection. Insurance card scanning, eligibility tools, and real-time verification reduce future denials. A strong patient access process directly improves clean claim rates and speeds up reimbursement.
Stage 2: Insurance Eligibility & Benefits Verification in US Healthcare RCM
Eligibility verification ensures the patient’s insurance is active, valid, and payable on the date of service. This step confirms coverage limits, co-pay amounts, deductibles, and prior authorization requirements.
In US Healthcare RCM, skipping eligibility checks leads to preventable denials. Automated eligibility tools integrated with clearinghouses help staff verify benefits in seconds. This stage protects providers from unpaid services and surprise write-offs.
Stage 3: Medical Coding in US Healthcare RCM
Medical coding converts clinical documentation into ICD-10, CPT, and HCPCS codes. Coding accuracy is the engine of clean claims in US Healthcare RCM.
Certified coders analyse provider notes to assign precise codes that reflect medical necessity. Under-coding causes revenue loss, while over-coding triggers audits and compliance risks. Accurate coding ensures claims pass payer edits and supports full reimbursement.
Stage 4: Charge Capture in US Healthcare RCM
Charge capture ensures all billable services are recorded, priced, and entered into the billing system. Missed charges directly equal lost revenue.
In US Healthcare RCM, automated charge capture tools reduce human error and ensure no service goes unbilled. Linking EHR documentation with billing systems improves charge accuracy and speeds up the billing cycle. This stage safeguards provider earnings.
Stage 5: Claim Creation & Scrubbing in US Healthcare RCM
Claim creation transforms coded data into standardized claim forms such as CMS-1500 or UB-04. Claim scrubbing then checks for errors before submission.
In US Healthcare RCM, scrubbing software identifies missing modifiers, invalid codes, payer-specific rules, and formatting errors. This powerful quality gate dramatically increases first-pass acceptance rates and prevents costly rework.
Stage 6: Claim Submission in US Healthcare RCM
Clean claims are submitted electronically through clearinghouses to insurance payers. Electronic Data Interchange (EDI) accelerates this process.
US Healthcare RCM depends heavily on timely submission. Delayed claims risk timely filing denials. Fast, accurate submission improves Days in Accounts Receivable (DAR) and stabilizes cash flow.
Stage 7: Claim Adjudication in US Healthcare RCM
Claim adjudication is the payer’s review process. The payer validates coverage, pricing, medical necessity, and policy compliance.
In US Healthcare RCM, claims can be paid, denied, reduced, or pended. Understanding payer behaviour helps billing teams proactively reduce denials. Strong documentation and coding directly influence adjudication outcomes.
Stage 8: Payment Posting in US Healthcare RCM
Once adjudicated, payments are issued via ERA (Electronic Remittance Advice) or paper EOBs. Payment posting records payer payments and patient responsibility.
Accurate payment posting in US Healthcare RCM is essential for financial reporting and follow-up. Errors here distort AR data and hide underpayments. Automated posting tools improve speed and accuracy.
Stage 9: Denial Management in US Healthcare RCM
Denials are inevitable, but poor denial management is optional. This stage identifies denial reasons, corrects errors, and submits appeals.
In US Healthcare RCM, denial analytics reveal root causes such as eligibility failures, coding errors, or authorization gaps. A proactive denial strategy converts lost revenue into recovered income.
Stage 10: Patient Billing & Collections in US Healthcare RCM
After insurance payment, remaining balances shift to the patient. Transparent billing statements and flexible payment options improve collection rates.
In US Healthcare RCM, patient-friendly billing reduces bad debt and improves satisfaction. Clear communication builds trust and accelerates self-pay recovery.
Conclusion: Why US Healthcare RCM Mastery Matters
US Healthcare RCM is not just billing—it is a strategic revenue engine. Every stage connects directly to cash flow, compliance, and financial stability. Providers who invest in strong front-end processes, accurate coding, clean claims, and proactive denial management achieve faster payments and sustainable growth. Mastering US Healthcare RCM transforms healthcare organizations from reactive to revenue-driven.
Reference URLs
- https://www.ahima.org
- https://www.cms.gov
- https://www.hfma.org
- https://www.aapc.com
- https://www.healthit.gov
https://dheeranworld.site/us-healthcare-rcm-process-end-to-end